Diving into the world of health and medicine often feels like deciphering another language. Especially when stumbling upon terms like 'Myelodysplastic Syndrome.' But, let's unravel this complex name and break it down into digestible pieces.
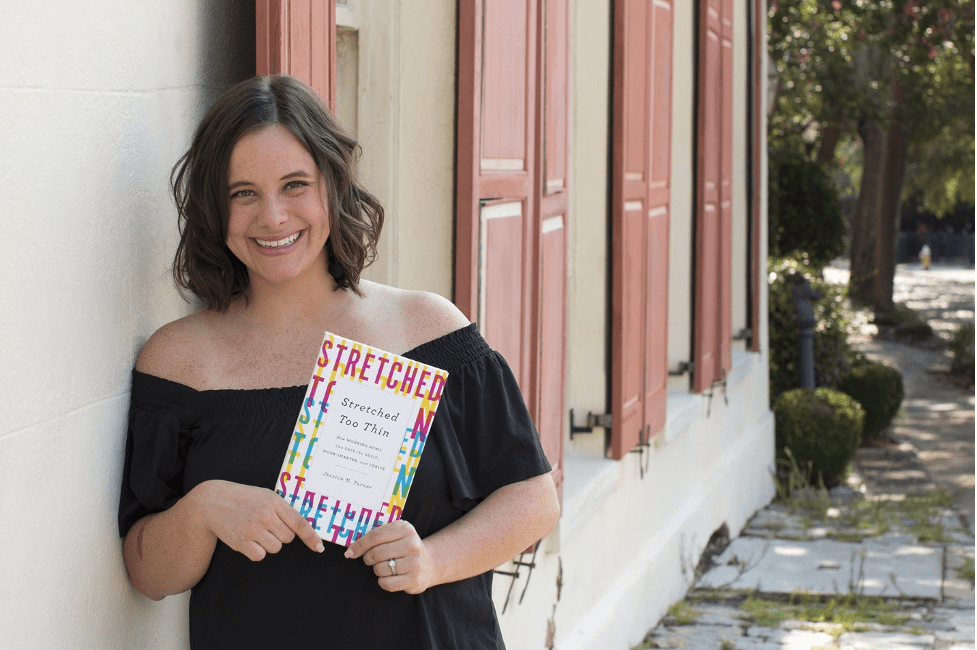
What is Myelodysplastic Syndrome?
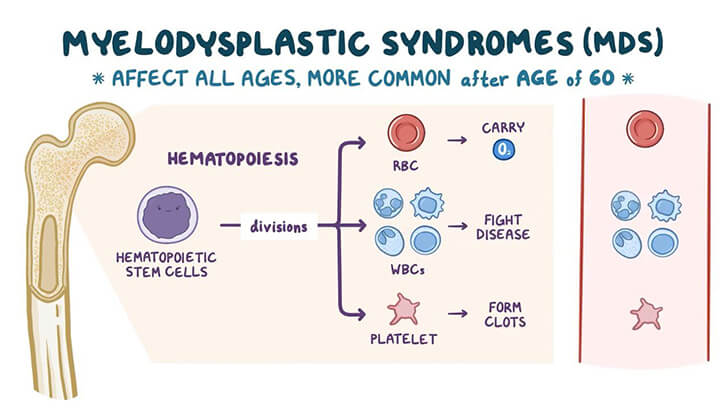
Osmosis.org
Myelodysplastic Syndrome (MDS), also known as myelodysplasia, refers to a group of disorders caused by poorly formed blood cells or ones that don't function correctly. Picture the bone marrow—our body's blood cell factory. In MDS, this factory produces faulty products, often leading to a decrease in healthy blood cells.
Types of Myelodysplasia
Refractory Cytopenia with Unilineage Dysplasia (RCUD)
This type is an umbrella term for MDS conditions where only one type (or lineage) of blood cell is primarily affected. The word "refractory" indicates that the cells are resistant to maturing properly.
Refractory anemia
This subtype is particularly concerned with the underproduction of red blood cells in the marrow, leading to fewer mature red cells in circulation. As a result, less oxygen is carried to the body's tissues, causing symptoms like fatigue and paleness.
Refractory neutropenia
This subtype affects the neutrophils, which are a type of white blood cell. Neutrophils are essential for fighting off bacterial infections. When their numbers dwindle, individuals are at a heightened risk for frequent and potentially severe infections.
Refractory thrombocytopenia
Here, the platelets are underproduced. Platelets are cell fragments that play a vital role in clotting. Without enough platelets, bleeding and bruising can become prominent issues.
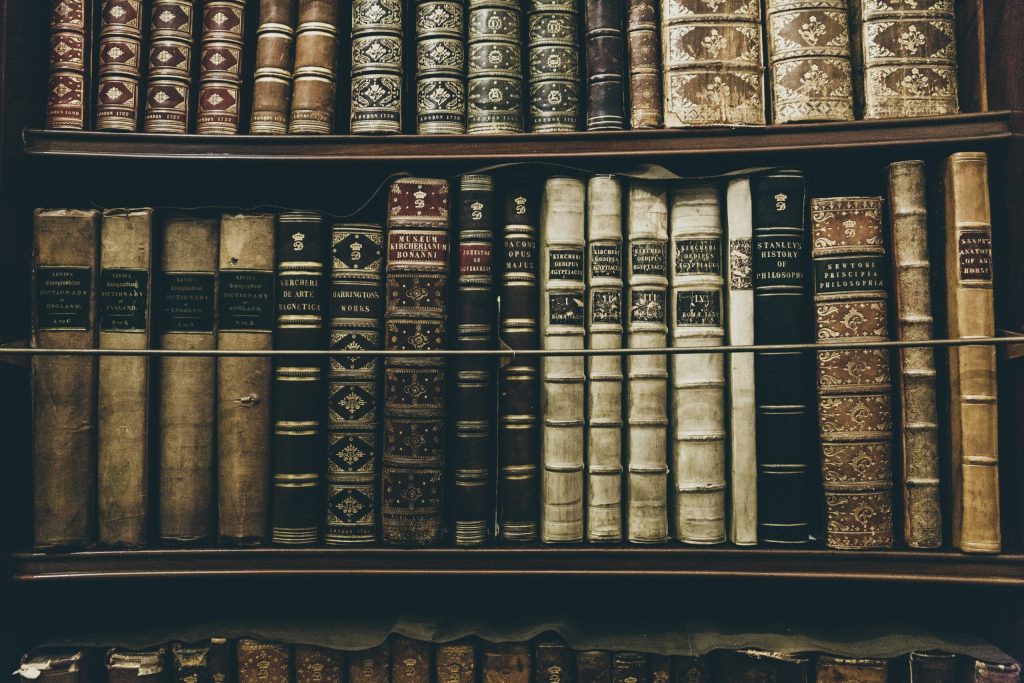
Refractory Anemia with Ringed Sideroblasts (RARS)
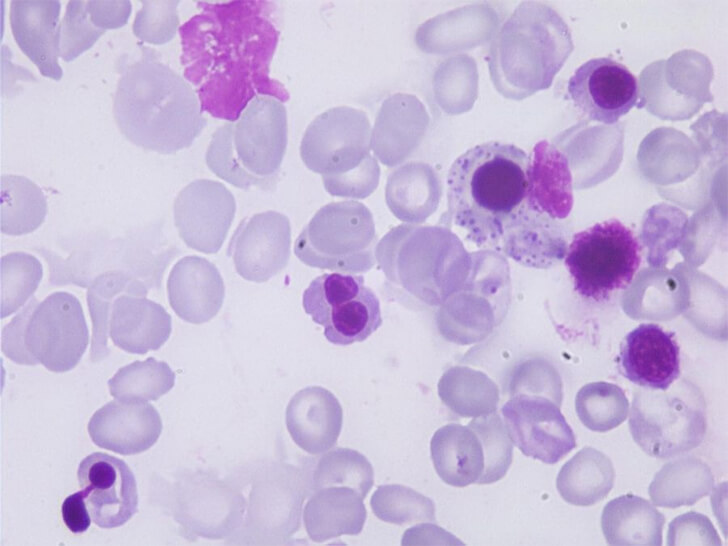
Atlas.Gechem.org
This type still concerns the red blood cells. However, the distinctive feature here is the accumulation of iron in mitochondria surrounding the nucleus of the developing red blood cells, resulting in what's termed "ringed sideroblasts" when viewed under a microscope. This iron buildup can impede the proper function of these cells, again leading to anemia-related symptoms.
Refractory Cytopenia with Multilineage Dysplasia (RCMD)
This is a more encompassing subtype of MDS, wherein two or more lineages of blood cells are dysplastic (abnormally developed). Due to its multi-lineage nature, the symptoms can be a combination of the aforementioned types, such as fatigue from anemia, susceptibility to infections due to low white blood cell count, and increased bleeding tendencies from reduced platelets.
Refractory Anemia with Excess Blasts (RAEB)
This subtype is characterized by an increased number of immature blood cells, called blasts, in the bone marrow. These blasts can crowd out healthy cells, leading to reduced production of mature cells. As the name suggests, the key concern here is the excess of these blasts. The subtype is further divided:
RAEB-1: Comprises 5-9% blasts in the bone marrow.
RAEB-2: Has between 10-19% blasts in the bone marrow. RAEB-2 is particularly concerning due to its higher potential of transforming into acute myeloid leukemia (AML), a more aggressive disease.
Chronic Myelomonocytic Leukemia (CMML)
CMML is a unique type as it blurs the lines between MDS and leukemia. It's marked by an elevated count of monocytes, another type of white blood cell, in the blood. These elevated counts can result in spleen enlargement, fevers, and weight loss. While it presents features of MDS, such as anemia, its progression, and complications can mirror that of leukemia.
Symptoms of Myelodysplastic Syndromes (MDS)

rawpixel.com / freepik
The manifestation of MDS symptoms often depends on the specific type of blood cell affected. As these syndromes can touch upon red blood cells, white blood cells, and platelets, the symptoms vary accordingly.
For red blood cells, which is a condition known as anemia, individuals may feel fatigued or weak. Paleness or pallor might be noticeable, coupled with shortness of breath. Some patients report dizziness, lightheadedness, chest pain, or palpitations.
If white blood cells are affected, the result can be frequent or prolonged infections. Sometimes, patients might have a fever with no obvious origin or experience unexpected weight loss.
When it comes to platelets, symptoms can manifest as easy bruising or small, pinpoint red marks on the skin known as petechiae. Patients may also observe prolonged bleeding from minor cuts, regular nosebleeds, or bleeding gums, especially after dental procedures or even simple activities like brushing.
Some individuals with MDS might experience other general symptoms, such as fever, loss of appetite, night sweats, or even bone pain.
Causes and Genetic Links of MDS

freepik / freepik
The genesis of MDS remains somewhat enigmatic, but certain factors are known to boost risk.
Exposure to specific chemicals, notably benzene and chemicals used in industries like petroleum and rubber, has been linked with MDS. Additionally, those who've undergone certain chemotherapy treatments or radiation for other cancers may later develop therapy-related MDS.
Genetics can also play a role. While the majority of MDS cases aren't inherited per se, some genetic syndromes like Fanconi anemia or Shwachman-Diamond syndrome do heighten the MDS risk. There are also certain chronic bone marrow disorders, such as chronic myeloproliferative disorder, that can predispose an individual to MDS. Age is another factor, with MDS appearing more predominantly in older adults.
On the topic of genetic mutations, a good number of MDS cases stem from mutations occurring within the bone marrow stem cells. Such mutations aren't passed down through families but occur throughout a person's life. Common mutations related to MDS include TP53, a gene acting as a tumor suppressor; genes like TET2, ASXL1, and DNMT3A, which play roles in cell development and differentiation; and genes such as SF3B1, SRSF2, U2AF1, and ZRSR2, impacting RNA splicing. Some patients may even harbor multiple mutations, and thanks to advances in medicine, it's now understood that certain mutations can offer insights into the disease's prognosis. This knowledge can pave the way for more personalized treatments.
Diagnosis Process
Diagnosing MDS involves a series of tests. A complete blood count (CBC) provides an initial clue, but the hallmark diagnostic procedure is a bone marrow biopsy. This test, though slightly uncomfortable, provides a clear picture of what's happening inside the bone marrow.
Treatment
MDS treatment is multifaceted and depends on the type, the patient's overall health, and the presence of specific genetic mutations. Options include supportive care (like blood transfusions), medications to increase blood cell count or treat the underlying disease, chemotherapy, or stem cell transplantation.
Self-Care with MDS

Drazen Zigic / freepik
Living with MDS demands a holistic approach. Maintaining a balanced diet, managing fatigue, regular health check-ups, and joining support groups can be beneficial. Avoiding infections by practicing good hygiene, like frequent hand-washing, and staying updated on vaccines is essential. Being aware of one's body, any new symptoms, or changes helps in managing the condition better.
In wrapping up this journey of understanding MDS, it's evident that while the name might seem daunting at first, getting acquainted with its intricacies makes it more navigable. Knowledge, as they say, is the first step to empowerment, especially when navigating the intricate paths of health and well-being.
show more